Endometriosis and Sex with Chantelle Otten
on 15 Sep 2022
This month, Chantelle Otten is giving us the run down on endometriosis, sex and why it's a bloody pain.

No one who gets their period looks forward to the cramps and mood swings. But imagine if your pain was so bad that you couldn’t get out of bed to go to the bathroom? Or had to go to the hospital for your period pain? Or if sex was causing you significant pain? These are some signs of endometriosis (A.K.A. endo).
For those who suffer from endo, periods can be excruciating. As you might know during your menstrual cycle, the lining of your uterus, the endometrium, builds up (to protect a fertilised egg) and sheds (when the egg is not fertilised).
Those who have endometriosis find this process super painful. Their periods can be crippling.
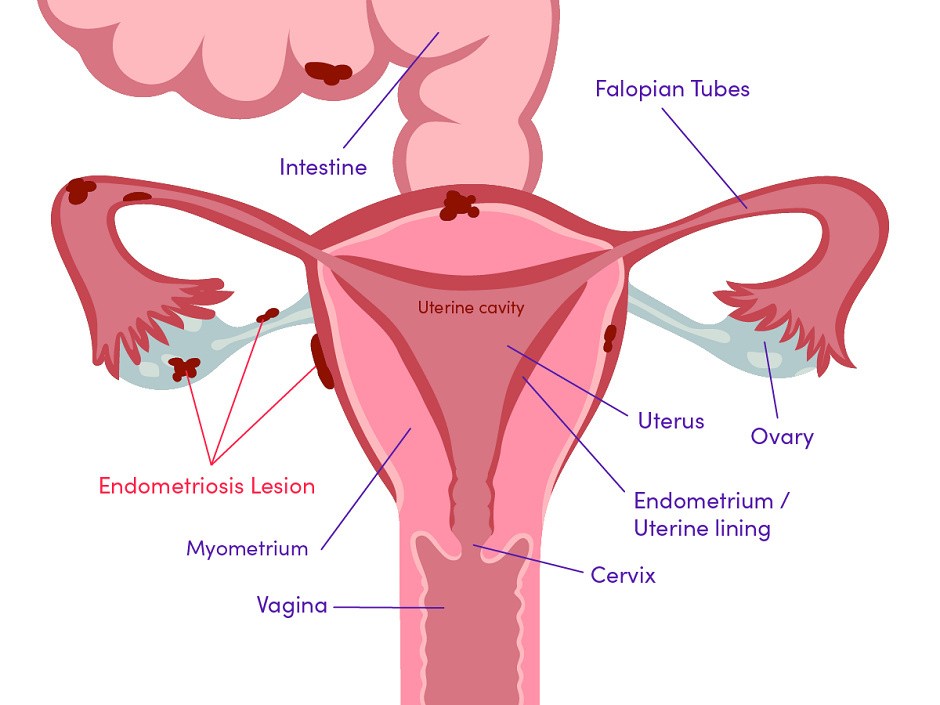
Why? Because for endo sufferers, cells that are similar to the lining which are meant to be inside the uterus actually grow outside of it, surrounding the ovaries and nearby areas. This builds up and breaks down and causes bleeding inside the pelvic floor, with corresponding pain, inflammation, swelling and scarring.
Now remember—and this is key—that endo (the condition) is not the endometrium! The endometrium is shed with our periods each month. But the cells causing endo don’t. They stay on the outside of the uterus, thickening each month, and getting more painful, and ultimately leading to adhesions (scar tissue that binds organs together) and endometriomas (sacs on the surface or inside the ovary that fill with old blood).
If these symptoms sound all too familiar to you, you are not alone. There are 176 million uterus owners worldwide who suffer from endo. That’s one in ten. So why isn’t it talked about more?
Often it takes between seven and ten years to get an endometriosis diagnosis, which sucks because it affects thousands of people, their livelihoods, their chances of having a baby and their sex lives.
If you think you or someone you care about might have endometriosis, here are a few signs to look out for (but know that some people have these signs while others have none):
Pain that begins before and continues into the period. Also lower back and abdominal pain.
Pain with penetration. Pain during and after sex is super common and may go hand in hand with other sexual pain conditions (such as vaginismus).
Pain doing a poo or peeing.
Lots of period blood and some bleeding in between periods.
Infertility. Sadly, a lot of people don’t realise they have endo until they are trying for a baby.
Other symptoms such as being super tired or having diarrhoea or constipation. Bloating or nausea is also common, usually with menstrual periods.
Pain and endo
Endometriosis can cause different types of pain, including chronic, long-lasting and really challenging pain. Some examples:
Dysmenorrhoea: painful menstruation, typically involving abdominal cramps.
Dyspareunia: difficult or painful vaginal intercourse (50 per cent to 79 per cent of patients)
Pain on penetration: vaginismus (40 per cent of patients). You may work with a physio who will recommend dilators to help desensitise the pelvic floor
Deeper pain
Post-coital pain: pain after penetrative sex (25 per cent to 50 per cent of patients)
Pelvic pain
Dyschezia: pain urinating/defecating

Sex and Endo
What elements of endometriosis affect sex? So many. There are physical and psychological aspects which come into play when endo is involved, alongside interpersonal relationships.
Physical
Pain in the pelvis, entrance of the cooch and deeper pain. You can use products such as the Lovehoney Health Penis Bumper set to make sure you don’t have a peen bumping a tender area.
Bowel-related pain associated with wind, bowel movements or diarrhoea
Rectal and anal pain with constipation
Painful urination
Backache and joint pain
Psychological
Depression
Anxiety
Lethargy and/or insomnia
Low self-esteem
Poor body image
Generally unwell feelings
Fatigue
Other sexual concerns with endometriosis
Almost 50 per cent of endo warriors struggle to have an orgasm (anorgasmia).
More than 50 per cent of endo sufferers have a loss of interest in sexual activity.

All of these aspects can lead to discomfort, fear of sex, low libido and performance anxiety. In fact, 40 per cent of endo patients suffer from vaginismus. Vaginismus is vaginal tightness causing discomfort, burning, pain, penetration problems or a complete inability to have vaginal intercourse.
For the partners, this can impact their confidence in being intimate with the endo sufferer, as they may not want to hurt them or know how best to approach them erotically.
How to Enjoy Intimacy with Endo
Positions are important here. Are there any positions you feel more comfortable in? Focus on enjoying these and adding in a vibrator to add extra pleasure to the experience.
Outercourse is also wonderful... I mean, you have a full body to play with! Penetration doesn't even need to be on the cards. Erotic massage, orgasmic meditation, clitoral vibrators, nipple play, ear nibbling... you name it!
Always lube up when it comes to any type of penetrative play, whether that be front door or back door. Silicone lube if using a penis, or water-based if using toys.
When it comes to getting help for endo, firstly, pick the right specialist. Now, it’s not your job to do this. Every doctor should be able to pick up endo symptoms . . . but unfortunately, this doesn’t always happen.
If you suspect you have endo, go see a gynaecologist who specialises in it. Do your research. You will most likely also need help from a pelvic floor physio and a sexologist.
Unfortunately, the only way to diagnose endo is through surgery, so be prepared that this may be suggested. Make sure your symptoms align before going through a procedure like this, even though it is generally very straightforward and minimally invasive.

Laparoscopy is the name of the surgery. Basically, the surgeon will make a tiny cut in your abdomen and insert a thin, lighted tube to take a small sample from the tissue and test it for endo. If it is endo tissue, they will usually remove it.
Endo is controlled with birth control and medication which stops the pituitary gland from releasing the hormone that makes the cells grow. There are a bunch of complementary treatments to help with endometriosis. Pelvic floor physiotherapy, pain management psychology, acupuncture and diet have all been shown to help ease the discomfort of the condition.
There are a bunch of complementary treatments to help with endometriosis as well. Pelvic floor physiotherapy, pain management psychology, acupuncture and diet have all been shown to help ease the discomfort of the condition.
For the general pain, warm Epsom salt baths, heating pads and TENS machines (an electronic medical device for transcutaneous electrical nerve stimulation) can also help an aching body and pelvic cramp.
Wherever you are on your endometriosis journey, it’s important to talk about it. We’ve got a long way to go in terms of research and treatment for this condition and as uterus owners, sharing our stories (if we’re comfortable to) and spreading awareness can have a great impact.
